This is a modified version of a press release originally written by Matt Shipman for NC State University.
Researchers have developed an inexpensive bandage that uses an electric field to promote healing in chronic wounds. In animal testing, wounds that were treated with these electric bandages healed 30% faster than wounds treated with conventional bandages.
Chronic wounds are open wounds that heal slowly, if they heal at all. For example, sores that occur in some patients with diabetes are chronic wounds. These wounds are particularly problematic because they often recur after treatment and significantly increase the risk of amputation and death.
One of the challenges associated with chronic wounds is that existing treatment options are extremely expensive, which can create additional problems for patients.
“Our goal here was to develop a far less expensive technology that accelerates healing in patients with chronic wounds,” says Amay Bandodkar, co-corresponding author of the work and an assistant professor of electrical and computer engineering at North Carolina State University. “We also wanted to make sure that the technology is easy enough for people to use at home, rather than something that patients can only receive in clinical settings.”
“This project is part of a bigger DARPA project to accelerate wound healing with personalized wound dressings,” says Sam Sia, co-corresponding author of the work and professor of biomedical engineering at Columbia University. “This collaborative project shows that these lightweight bandages, which can provide electrical stimulation simply by adding water, healed wounds faster than the control, at a similar rate as bulkier and more expensive wound treatment.”
The research team includes experts from NC State, Columbia Engineering, Beth Israel Deaconess Medical Center, the joint biomedical engineering program at NC State and the University of North Carolina at Chapel Hill, Korea University, Georgia Tech, and the Korea Institute of Science and Technology.
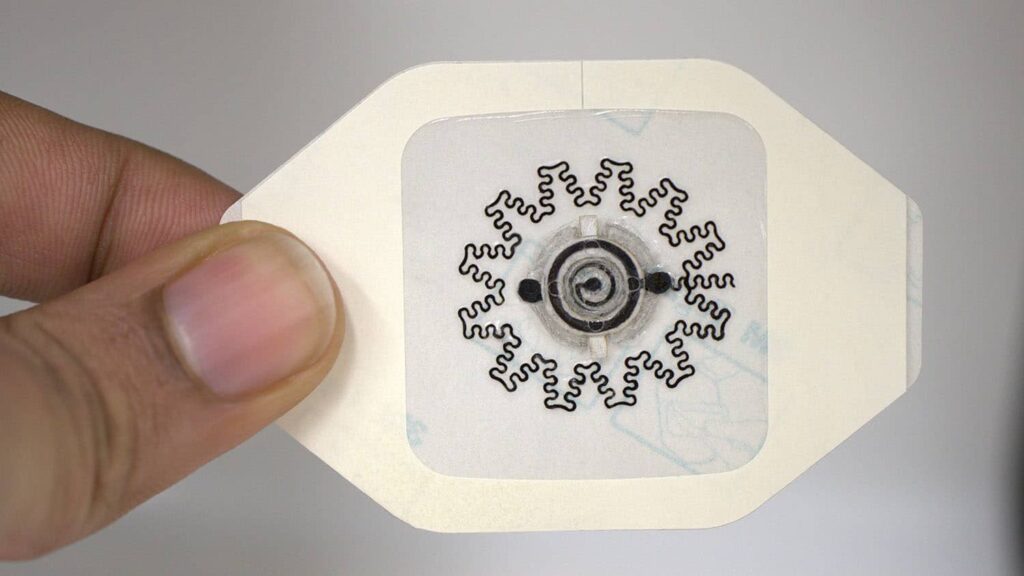
Specifically, the research team developed water-powered, electronics-free dressings (WPEDs), which are disposable wound dressings that have electrodes on one side and a small, biocompatible battery on the other. The dressing is applied to a patient so that the electrodes come into contact with the wound. A drop of water is then applied to the battery, activating it. Once activated, the bandage produces an electric field for several hours.
“That electric field is critical, because it’s well established that electric fields accelerate healing in chronic wounds,” says Rajaram Kaveti, co-first author of the study and a post-doctoral researcher at NC State.
The electrodes are designed in a way that allows them to bend with the bandage and conform to the surface of the chronic wounds, which are often deep and irregularly shaped.
“This ability to conform is critical, because we want the electric field to be directed from the periphery of the wound toward the wound’s center,” says Kaveti. “In order to focus the electric field effectively, you want electrodes to be in contact with the patient at both the periphery and center of the wound itself. And since these wounds can be asymmetrical and deep, you need to have electrodes that can conform to a wide variety of surface features.”
“We tested the wound dressings in diabetic mice, which are a commonly used model for human wound healing,” says Maggie Jakus, co-first author of the study and a graduate student at Columbia. “We found that the electrical stimulation from the device sped up the rate of wound closure, promoted new blood vessel formation, and reduced inflammation, all of which point to overall improved wound healing.”
Specifically, the researchers found that mice who received treatment with WPEDs healed about 30% faster than mice who received conventional bandages.
“But it is equally important that these bandages can be produced at relatively low cost – we’re talking about a couple of dollars per dressing in overhead costs.” says Bandodkar.
“Diabetic foot ulceration is a serious problem that can lead to lower extremity amputations,” says Aristidis Veves, a co-author of the study and professor of surgery at Beth Israel Deaconess Center. “There is urgent need for new therapeutic approaches, as the last one that was approved by the Food and Drug Administration was developed more than 25 years ago. My team is very lucky to participate in this project that investigates innovative and efficient new techniques that have the potential to revolutionize the management of diabetic foot ulcers.”
In addition, the WPEDs can be applied quickly and easily. And once applied, patients can move around and take part in daily activities. This functionality means that patients can receive treatment at home and are more likely to comply with treatment. In other words, patients are less likely to skip treatment sessions or take shortcuts, since they aren’t required to come to a clinic or remain immobile for hours.
“Next steps for us include additional work to fine-tune our ability to reduce fluctuations in the electric field and extend the duration of the field. We are also moving forward with additional testing that will get us closer to clinical trials and – ultimately – practical use that can help people,” says Bandodkar.
The paper, “Water-powered, electronics-free dressings that electrically stimulate wounds for rapid wound closure,” is published in the open-access journal Science Advances. The paper’s co-authors include Henry Chen, an undergraduate in the joint biomedical engineering department at NC State and UNC; Bhavya Jain, Navya Mishra, Nivesh Sharma and Baha Erim Uzunoğlu, Ph.D. students at NC State; Darragh Kennedy and Elizabeth Caso of Columbia; Georgios Theocharidis and Brandon Sumpio of Beth Israel Deaconess Medical Center; Won Bae Han of Korea University and the Georgia Institute of Technology; Tae-Min Jang of Korea University; and Suk-Won Hwang of Korea University and the Korea Institute of Science and Technology.
This work was done with support from the Defense Advanced Research Projects Agency under grant D20AC00004 and from the ASSIST Center (Center for Advanced Self-Powered Systems of Integrated Sensors and Technologies) at NC State, which is funded by National Science Foundation grant 1160483. Bandodkar and Kaveti are inventors on a patent application related to this work.
